How to talk to your GP about menstrual pain
For many of us, menstrual pain is a monthly challenge that can greatly impact our daily life. Often, we're unsure about how to talk to our GP about menstrual pain or even how to measure the intensity of the pain in a way that can be articulated in our appointments.
Why see the GP for menstrual pain?
- To rule out any underlying conditions - the GP can check your general health and refer you, for example, for a scan so you can both see what's going on
- To get all the options for prescription medication for pain management
- To discuss lifestyle changes, for example, diet and exercise. You can ask your GP about what's available locally on social prescription to support these.
Severe menstrual pain is not something that you should have to experience silently or alone. It can be a symptom of underlying conditions like endometriosis or fibroids requiring medical attention.
Sharing your experiences with your GP allows them to identify any potential issues and propose appropriate treatment. Your GP can provide valuable advice on managing pain and improving your quality of life during your menstrual cycle.
Remember: menstrual pain is a valid and significant health concern, and it deserves the full attention of your healthcare provider.
In this blog, we will guide you through discussing menstrual pain with your GP - from understanding its causes and misconceptions to learning how to communicate your pain levels and symptoms effectively.
We also offer a free, clinically-backed menstrual cycle support course to help you navigate this journey more confidently. Let's start by demystifying menstrual pain, so you can discuss it openly and receive the care you deserve.

Definition and causes of menstrual pain
Menstrual pain, or dysmenorrhea, is the abdominal cramping and/or lower back pain that some women experience before and during their period. This can range from mild to severe in intensity, but it's usually not dangerous.
Menstrual pain is caused by increased prostaglandins - hormones that help the uterus contract to shed its lining. When levels of these hormones are high, the uterus contracts more strongly and causes pain.
It's important to understand that not all women experience menstrual pain - some do not feel any discomfort at all! But for those who do, it can range from mild cramps to intense pain that disrupts everyday activities.
Common misconceptions about menstrual pain
There are a few misconceptions about menstrual pain that can be discouraging to women who experience it.
Firstly, many people think that all menstrual pain is the same and should be able to be managed with over-the-counter medications like ibuprofen. However, these medications only work for mild symptoms - if you're experiencing more intense pain, it's best to speak to your GP for a tailored plan.
Secondly, some people assume that all menstrual pain is normal and that medical attention is unnecessary. This is not true - severe or prolonged menstrual pain can indicate an underlying condition and should always be discussed with your doctor.
Finally, many women are hesitant to discuss menstrual pain in fear of being judged or dismissed. Remember: your GP is there to listen and provide support.
Research has shown that when women are comfortable talking openly about their menstrual health, they're more likely to receive the treatment they need for any underlying issues.

Measuring Menstrual Pain
It can be hard to accurately gauge the severity of your menstrual pain and how it compares with other people's experiences. Even amongst friends and peers, the intensity of menstrual pain is not always accurately represented. For instance, some may downplay their symptoms while others overstate or exaggerate them.
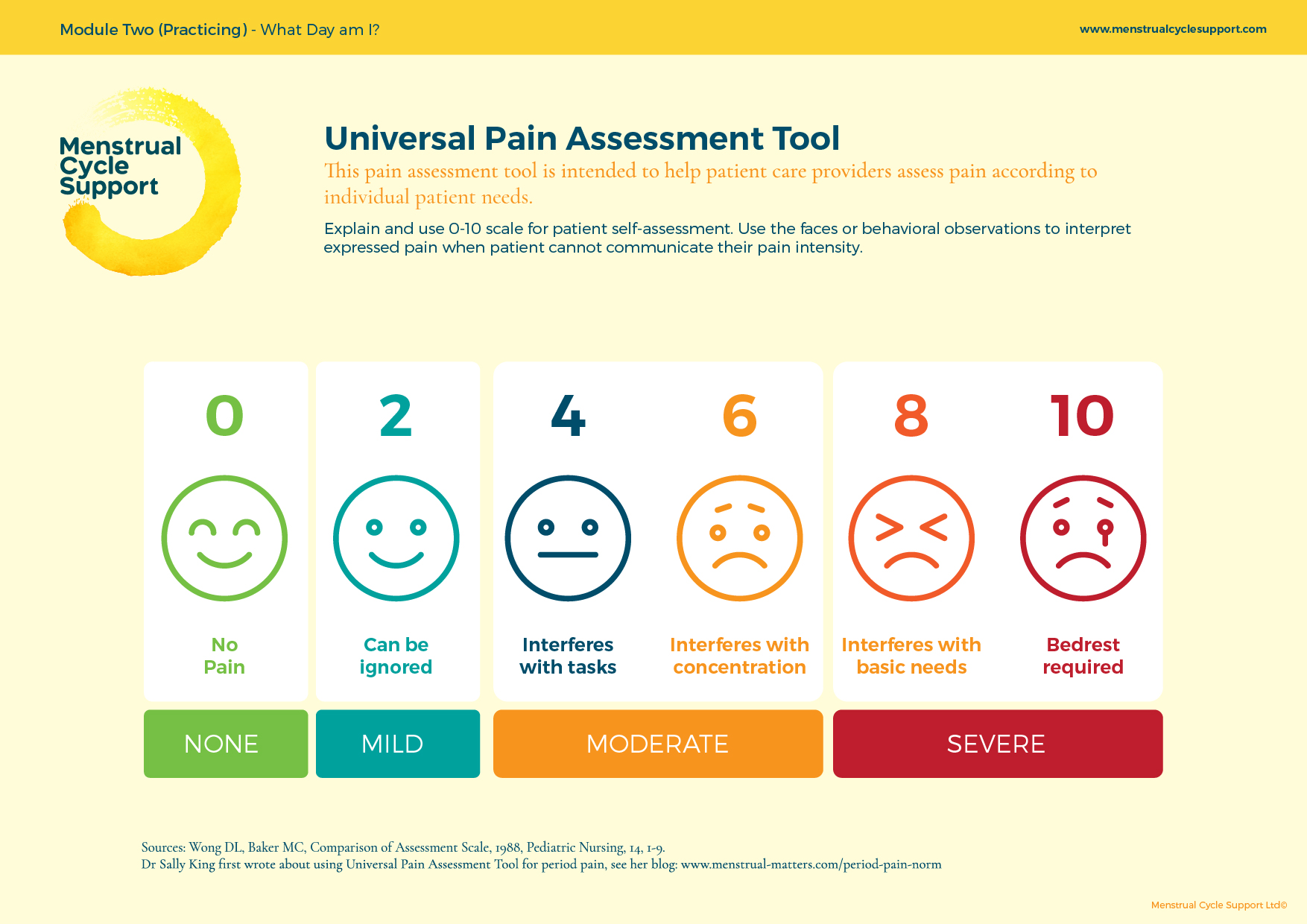
The Universal Pain Scale is a commonly used tool in medical settings that can be very helpful in expressing menstrual pain. It uses a simple numerical system to help you identify and communicate the level of your discomfort to your healthcare provider.
As part of our free, clinically-backed menstrual cycle support course, we provide comprehensive guidance on how to use this tool effectively. We believe that by using the Universal Pain Scale, you can accurately articulate the extent of your menstrual pain to your GP. This vital communication can greatly assist your GP in providing the correct diagnosis and the most effective pain management strategies.
Remember, your pain is personal, and the scale is subjective - what might be a 3 for you could be a 7 for someone else.
The important thing is that you can relay your experiences of pain in a way that helps your GP understand the full extent of your discomfort. With the Universal Pain Scale, you'll have a consistent method to gauge your pain levels and communicate your needs effectively.
Keeping track of menstrual pain symptoms
Charting your menstrual cycle can empower you to better understand your body and how it functions. Not only does it help you predict when your periods will start, but it also sheds light on your unique patterns of menstrual pain.
This knowledge can make it easier to plan your daily activities around your cycle and better manage any discomfort you may experience. Keeping track of your menstrual cycle can be a valuable tool when discussing your menstrual pain with your GP.
By giving your GP a detailed picture of your cycle, it can help them provide a more accurate diagnosis, and tailor a treatment plan that's best suited to your individual needs.
Charting your menstrual cycle encourages a more proactive approach to your health. By getting familiar with your body's rhythms and signals, you can be better prepared to spot any sudden changes or anomalies that may need medical attention.
When charting your menstrual cycle, consider noting the following:
- Start and end dates of your period
- Severity of menstrual pain on each day of your period, rated on a scale from 1-10
- Any associated symptoms such as bloating, nausea, fatigue, or mood swings
- Changes in the heaviness of bleeding
- Non-menstrual symptoms, such as ovulation pain or changes in cervical mucus
- Any lifestyle factors that could be impacting your cycle, such as stress, diet, or exercise.
- Taking the time to chart your menstrual cycle can be an empowering step in your journey towards understanding and managing your menstrual health.
- Remember, your experience with menstrual pain is personal and unique to you. There's no need to compare your symptoms with others, and there's no such thing as a 'normal' cycle. Understanding your own cycle is the most important thing.

5 Tips for Talking to your GP about your menstrual pain
Opening up about personal health matters can be challenging, especially when it comes to menstrual pain.
Many people struggle to describe their symptoms and their impact on their life, leaving them feeling unheard or misunderstood.
1. Be Honest and Open
Speak truthfully about your experiences, symptoms, and the level of discomfort you're feeling. Do not downplay or exaggerate your pain. Your GP's understanding of your situation is crucial to providing the right advice and treatment.
2. Use the Universal Pain Tool
Rate your menstrual pain on a scale of 1-10, with 1 being mild and 10 being the worst pain you've ever felt. This gives your GP a more tangible understanding of your discomfort
3. Chart Your Symptoms
Keep a record of your symptoms throughout the month, noting any changes or patterns and try to do this for 2-3 cycles. This could help reveal potential underlying conditions and aids in providing a comprehensive picture to your GP.
4. Mention the Impact on Daily Life
Discuss how menstrual pain is affecting your day-to-day life. This includes any activities you've had to avoid or changes in your work or personal life due to your symptoms.
5. Ask Questions
Don't hesitate to ask your GP any questions or voice any concerns you might have. The more you understand about your condition, the better you can manage it. Remember, your GP is there to help you.

Discussing Treatment Options
Once your GP has evaluated your symptoms, they may suggest various treatment options. This could include lifestyle changes such as exercise or dietary modifications, medications to help manage pain and discomfort, or further investigation into potential underlying conditions.
Be sure to discuss your concerns with your GP before deciding on treatment. It is important to remember that each treatment option carries its own risks and benefits. Weighing the pros and cons with your GP is important in finding the best approach to managing your menstrual pain.
Finally, if you're feeling lost or overwhelmed by all of this information, don't forget to take a look at our free menstrual cycle support course — it's full of useful resources to help you better understand and manage menstrual pain.
Free Menstrual Cycle Pain Resources
Understanding and managing menstrual pain requires open dialogue with your GP, personal observation, and effective tracking of symptoms.
Remember, it's vital to ask questions, seek clarification, and express any concerns you have about your menstrual health. The journey to better menstrual health management is unique to each individual, and there's no one-size-fits-all solution.
We highly recommend signing up for our free, clinically-backed menstrual cycle support course to further support your journey.
This course offers comprehensive resources to help you better understand menstrual pain and effective ways to manage it. Take charge of your menstrual health today by enrolling in the course.
